Dr Sergey Bromberg
- General practice
- Fee: $59

Dr Noah Verderio
- General practice
- Fee: $59

Aatisha
- General practice
- Fee: $10

Dr Roger Wank
- General practice
- Fee: $49
What Other People are Saying
Grab a look at our outstanding and stunning My Farmacy App feedback which is given by our satisfied customers.
Stories, Tips & Latest News
It is a long established fact that a reader will be distracted by the readable content of a page when looking at its layout.
How medicinal plants changed the world
Introduction and Importance of Medicinal Plants and HerbsIntroductionThe term “medicinal plant” include various types of plants used in herbalism ("herbology" or "herbal medicine"). It is the use of plants for medicinal purposes, and the study of such uses.The word “herb” has been derived from the Latin word, “herba” and an old French word “herbe”.Now a days, herb refers to any part of the plant like fruit, seed, stem, bark, flower, leaf, stigma or a root, as well as a non-woody plant. Earlier, the term “herb” was only applied to non-woody plants, including those that come from trees and shrubs. These medicinal plants are also used as food, flavonoid, medicine or perfume and also in certain spiritual activities.Plants have been used for medicinal purposes long before prehistoric period. Ancient Unani manuscripts Egyptian papyrus and Chinese writings described the use of herbs. Evidence exist that Unani Hakims, Indian Vaids and European and Mediterranean cultures were using herbs for over 4000 years as medicine. Indigenous cultures such as Rome, Egypt, Iran, Africa and America used herbs in their healing rituals, while other developed traditional medical systems such as Unani, Ayurveda and Chinese Medicine in which herbal therapies were used systematically.Traditional systems of medicine continue to be widely practised on many accounts. Population rise, inadequate supply of drugs, prohibitive cost of treatments, side effects of several synthetic drugs and development of resistance to currently used drugs for infectious diseases have led to increased emphasis on the use of plant materials as a source of medicines for a wide variety of human ailments.Among ancient civilisations, India has been known to be rich repository of medicinal plants. The forest in India is the principal repository of large number of medicinal and aromatic plants, which are largely collected as raw materials for manufacture of drugs and perfumery products. About 8,000 herbal remedies have been codified in AYUSH systems in INDIA. Ayurveda, Unani, Siddha and Folk (tribal) medicines are the major systems of indigenous medicines. Among these systems, Ayurveda and Unani Medicine are most developed and widely practised in India.Recently, WHO (World Health Organization) estimated that 80 percent of people worldwide rely on herbal medicines for some aspect of their primary health care needs. According to WHO, around 21,000 plant species have the potential for being used as medicinal plants.As per data available over three-quarters of the world population relies mainly on plants and plant extracts for their health care needs. More than 30% of the entire plant species, at one time or other were used for medicinal purposes. It has been estimated, that in developed countries such as United States, plant drugs constitute as much as 25% of the total drugs, while in fast developing countries such as India and China, the contribution is as much as 80%. Thus, the economic importance of medicinal plants is much more to countries such as India than to rest of the world. These countries provide two third of the plants used in modern system of medicine and the health care system of rural population depend on indigenous systems of medicine.Treatment with medicinal plants is considered very safe as there is no or minimal side effects. These remedies are in sync with nature, which is the biggest advantage. The golden fact is that, use of herbal treatments is independent of any age groups and the sexes.The ancient scholars only believed that herbs are only solutions to cure a number of health related problems and diseases. They conducted thorough study about the same, experimented to arrive at accurate conclusions about the efficacy of different herbs that have medicinal value. Most of the drugs, thus formulated, are free of side effects or reactions. This is the reason why herbal treatment is growing in popularity across the globe. These herbs that have medicinal quality provide rational means for the treatment of many internal diseases, which are otherwise considered difficult to cure.Medicinal plants such as Aloe, Tulsi, Neem, Turmeric and Ginger cure several common ailments. These are considered as home remedies in many parts of the country. It is known fact that lots of consumers are using Basil (Tulsi) for making medicines, black tea, in pooja and other activities in their day to day life.In several parts of the world many herbs are used to honour their kings showing it as a symbol of luck. Now, after finding the role of herbs in medicine, lots of consumers started the plantation of tulsi and other medicinal plants in their home gardens.Medicinal plants are considered as a rich resources of ingredients which can be used in drug development either pharmacopoeial, non- pharmacopoeial or synthetic drugs. A part from that, these plants play a critical role in the development of human cultures around the whole world. Moreover, some plants are considered as important source of nutrition and as a result of that they are recommended for their therapeutic values. Some of these plants include ginger, green tea, walnuts, aloe, pepper and turmeric etc. Some plants and their derivatives are considered as important source for active ingredients which are used in aspirin and toothpaste etc.Apart from the medicinal uses, herbs are also used in natural dye, pest control, food, perfume, tea and so on. In many countries different kinds of medicinal plants/ herbs are used to keep ants, flies, mice and flee away from homes and offices. Now a days medicinal herbs are important sources for pharmaceutical manufacturing.Recipes for the treatment of common ailments such as diarrhoea, constipation, hypertension, low sperm count, dysentery and weak penile erection, piles, coated tongue, menstrual disorders, bronchial asthma, leucorrhoea and fevers are given by the traditional medicine practitioners very effectively.Over the past two decades, there has been a tremendous increase in the use of herbal medicine; however, there is still a significant lack of research data in this field. Therefore since 1999, WHO has published three volumes of the WHO monographs on selected medicinal plants.Importance of some herbs with their medicinal valuesHerbs such as black pepper, cinnamon, myrrh, aloe, sandalwood, ginseng, red clover, burdock, bayberry, and safflower are used to heal wounds, sores and boils.Basil, Fennel, Chives, Cilantro, Apple Mint, Thyme, Golden Oregano, Variegated Lemon Balm, Rosemary, Variegated Sage are some important medicinal herbs and can be planted in kitchen garden. These herbs are easy to grow, look good, taste and smell amazing and many of them are magnets for bees and butterflies.Many herbs are used as blood purifiers to alter or change a long-standing condition by eliminating the metabolic toxins. These are also known as 'blood cleansers'. Certain herbs improve the immunity of the person, thereby reducing conditions such as fever.Some herbs are also having antibiotic properties. Turmeric is useful in inhibiting the growth of germs, harmful microbes and bacteria. Turmeric is widely used as a home remedy to heal cut and wounds.To reduce fever and the production of heat caused by the condition, certain antipyretic herbs such as Chirayta, black pepper, sandal wood and safflower are recommended by traditional Indian medicine practitioners.Sandalwood and Cinnamon are great astringents apart from being aromatic. Sandalwood is especially used in arresting the discharge of blood, mucus etc.Some herbs are used to neutralize the acid produced by the stomach. Herbs such as marshmallow root and leaf. They serve as antacids. The healthy gastric acid needed for proper digestion is retained by such herbs.Indian sages were known to have remedies from plants which act against poisons from animals and snake bites.Herbs like Cardamom and Coriander are renowned for their appetizing qualities. Other aromatic herbs such as peppermint, cloves and turmeric add a pleasant aroma to the food, thereby increasing the taste of the meal.Some herbs like aloe, sandalwood, turmeric, sheetraj hindi and khare khasak are commonly used as antiseptic and are very high in their medicinal values.Ginger and cloves are used in certain cough syrups. They are known for their expectorant property, which promotes the thinning and ejection of mucus from the lungs, trachea and bronchi. Eucalyptus, Cardamom, Wild cherry and cloves are also expectorants.Herbs such as Chamomile, Calamus, Ajwain, Basil, Cardamom, Chrysanthemum, Coriander, Fennel, Peppermint and Spearmint, Cinnamon, Ginger and Turmeric are helpful in promoting good blood circulation. Therefore, they are used as cardiac stimulants.Certain medicinal herbs have disinfectant property, which destroys disease causing germs. They also inhibit the growth of pathogenic microbes that cause communicable diseases.Herbal medicine practitioners recommend calmative herbs, which provide a soothing effect to the body. They are often used as sedatives.Certain aromatic plants such as Aloe, Golden seal, Barberry and Chirayata are used as mild tonics. The bitter taste of such plants reduces toxins in blood. They are helpful in destroying infection as well.Certain herbs are used as stimulants to increase the activity of a system or an organ, for example herbs like Cayenne (Lal Mirch, Myrrh, Camphor and Guggul. A wide variety of herbs including Giloe, Golden seal, Aloe and Barberry are used as tonics. They can also be nutritive and rejuvenate a healthy as well as diseased individual.Honey, turmeric, marshmallow and liquorice can effectively treat a fresh cut and wound. They are termed as vulnerary herbs.ConclusionAs our lifestyle is now getting techno-savvy, we are moving away from nature. While we cannot escape from nature because we are part of nature. As herbs are natural products they are free from side effects, they are comparatively safe, eco-friendly and locally available. Traditionally there are lot of herbs used for the ailments related to different seasons. There is a need to promote them to save the human lives.These herbal products are today are the symbol of safety in contrast to the synthetic drugs, that are regarded as unsafe to human being and environment. Although herbs had been priced for their medicinal, flavouring and aromatic qualities for centuries, the synthetic products of the modern age surpassed their importance, for a while. However, the blind dependence on synthetics is over and people are returning to the naturals with hope of safety and security. It’s time to promote them globally.
Read MoreMedical Cannabis for Chronic Pain: Analysis
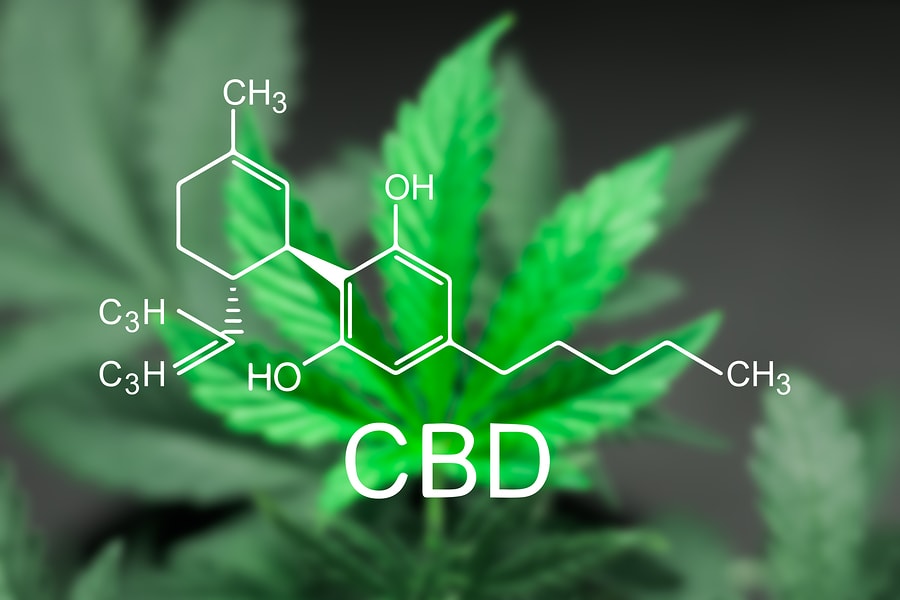
Therapeutic Effects of Cannabis and CannabinoidsPublication DetailsChapter HighlightsIn adults with chemotherapy-induced nausea and vomiting, oral cannabinoids are effective antiemetics.In adults with chronic pain, patients who were treated with cannabis or cannabinoids are more likely to experience a clinically significant reduction in pain symptoms.In adults with multiple sclerosis (MS)-related spasticity, short-term use of oral cannabinoids improves patient-reported spasticity symptoms.For these conditions the effects of cannabinoids are modest; for all other conditions evaluated there is inadequate information to assess their effects.Cannabis sativa has a long history as a medicinal plant, likely dating back more than two millennia (Russo et al., 2007). It was available as a licensed medicine in the United States for about a century before the American Medical Association removed it from the 12th edition of the U.S. Pharmacopeia (IOM, 1999). In 1985, pharmaceutical companies received approval to begin developing Δ9-tetrahydrocannabinol (THC) preparations—dronabinol and nabilone—for therapeutic use, and as a result, cannabinoids were reintroduced into the armamentarium of willing health care providers (Grotenhermen and Müller-Vahl, 2012). Efforts are now being put into the trials of cannabidiol as a treatment for conditions such as epilepsy and schizophrenia,1 although no such preparations have come to market at this time. Nabiximols, an oromucosal spray of a whole cannabis plant extract with a 1:1 ratio of THC to cannabidiol (CBD), was initially licensed and approved in Europe, the United Kingdom, and Canada for the treatment of pain and spasticity associated with multiple sclerosis (GW Pharmaceuticals, 2016; Pertwee, 2012), but it continues to undergo evaluation in Phase III clinical trials in the United States.2 Efforts are under way to develop targeted pharmaceuticals that are agonists or antagonists of the cannabinoid receptors or that modulate the production and degradation of the endocannabinoids, although such interventions have not yet demonstrated safety or effectiveness. Nonetheless, therapeutic agents targeting cannabinoid receptors and endocannabinoids are expected to become available in the future.The renewed interest in the therapeutic effects of cannabis emanates from the movement that began 20 years ago to make cannabis available as a medicine to patients with a variety of conditions. It was in 1996 that Arizona and California first passed medicinal cannabis legislation, although Arizona later rescinded the approval, so it would be California that paved the way. At the time that this report was written, in 2016, 28 states and the District of Columbia had legalized the medical use of cannabis; 8 states had legalized both medical and recreational use of cannabis; and another 16 states had allowed limited access to low-THC/high-CBD products (i.e., products with low levels of THC and high levels of CBD) (NCSL, 2016). A recent national survey showed that among current adult users, 10.5 percent reported using cannabis solely for medical purposes, and 46.6 percent reported a mixed medical/recreational use (Schauer et al., 2016). Of the states that allow for some access to cannabis compounds, cancer, HIV/AIDS, multiple sclerosis, glaucoma, seizures/epilepsy, and pain are among the most recognized qualifying ailments (Belendiuk et al., 2015; NCSL, 2016). There are certain states that provide more flexibility than others and that allow the use of medical cannabis for the treatment of any illness for which the drug provides relief for the individual. Given the steady liberalization of cannabis laws, the numbers of these states are likely to increase and therefore support the efforts to clarify the potential therapeutic benefits of medical cannabis on various health outcomes.For example, the most common conditions for which medical cannabis is used in Colorado and Oregon are pain, spasticity associated with multiple sclerosis, nausea, posttraumatic stress disorder, cancer, epilepsy, cachexia, glaucoma, HIV/AIDS, and degenerative neurological conditions (CDPHE, 2016; OHA, 2016). We added to these conditions of interest by examining lists of qualifying ailments in states where such use is legal under state law. The resulting therapeutic uses covered by this chapter are chronic pain, cancer, chemotherapy-induced nausea and vomiting, anorexia and weight loss associated with HIV, irritable bowel syndrome, epilepsy, spasticity, Tourette syndrome, amyotrophic lateral sclerosis, Huntington's disease, Parkinson's disease, dystonia, dementia, glaucoma, traumatic brain injury, addiction, anxiety, depression, sleep disorders, posttraumatic stress disorder, and schizophrenia and other psychoses. The committee is aware that there may be other conditions for which there is evidence of efficacy for cannabis or cannabinoids. In this chapter, the committee will discuss the findings from 16 of the most recent, good- to fair-quality systematic reviews and 21 primary literature articles that best address the committee's research questions of interest.As a reminder to the reader, several of the prioritized health endpoints discussed here in Part II are also reviewed in chapters of Part III; however, the research conclusions within these chapters may differ. This is, in part, due to differences in the study design of the evidence reviewed (e.g., randomized controlled trials [RCTs] versus epidemiological studies), differences in the characteristics of cannabis or cannabinoid exposure (e.g., form, dose, frequency of use), and the populations studied. As such, it is important that the reader is aware that this report was not designed to reconcile the proposed harms and benefits of cannabis or cannabinoid use across chapters.CHRONIC PAINRelief from chronic pain is by far the most common condition cited by patients for the medical use of cannabis. For example, Light et al. (2014) reported that 94 percent of Colorado medical marijuana ID cardholders indicated “severe pain” as a medical condition. Likewise, Ilgen et al. (2013)reported that 87 percent of participants in their study were seeking medical marijuana for pain relief. In addition, there is evidence that some individuals are replacing the use of conventional pain medications (e.g., opiates) with cannabis. For example, one recent study reported survey data from patrons of a Michigan medical marijuana dispensary suggesting that medical cannabis use in pain patients was associated with a 64 percent reduction in opioid use (Boehnke et al., 2016). Similarly, recent analyses of prescription data from Medicare Part D enrollees in states with medical access to cannabis suggest a significant reduction in the prescription of conventional pain medications (Bradford and Bradford, 2016). Combined with the survey data suggesting that pain is one of the primary reasons for the use of medical cannabis, these recent reports suggest that a number of pain patients are replacing the use of opioids with cannabis, despite the fact that cannabis has not been approved by the U.S. Food and Drug Administration (FDA) for chronic pain.Are Cannabis or Cannabinoids an Effective Treatment for the Reduction of Chronic Pain?Systematic ReviewsFive good- to fair-quality systematic reviews were identified. Of those five reviews, Whiting et al. (2015) was the most comprehensive, both in terms of the target medical conditions and in terms of the cannabinoids tested. Snedecor et al. (2013)was narrowly focused on pain related to spinal cord injury, did not include any studies that used cannabis, and only identified one study investigating cannabinoids (dronabinol). Two reviews on pain related to rheumatoid arthritis did not contribute unique studies or findings (Fitzcharles et al., 2016; Richards et al., 2012). Finally, one review (Andreae et al., 2015) conducted a Bayesian analysis of five primary studies of peripheral neuropathy that had tested the efficacy of cannabis in flower form administered via inhalation. Two of the primary studies in that review were also included in the Whiting review, while the other three were not. It is worth noting that the conclusions across all of the reviews were largely consistent in suggesting that cannabinoids demonstrate a modest effect on pain. For the purposes of this discussion, the primary source of information for the effect on cannabinoids on chronic pain was the review by Whiting et al. (2015). Whiting et al. (2015) included RCTs that compared cannabinoids to usual care, a placebo, or no treatment for 10 conditions. Where RCTs were unavailable for a condition or outcome, nonrandomized studies, including uncontrolled studies, were considered. This information was supplemented by a search of the primary literature from April 2015 to August 2016 as well as by additional context from Andreae et al. (2015) that was specific to the effects of inhaled cannabinoids.The rigorous screening approach used by Whiting et al. (2015) led to the identification of 28 randomized trials in patients with chronic pain (2,454 participants). Twenty-two of these trials evaluated plant-derived cannabinoids (nabiximols, 13 trials; plant flower that was smoked or vaporized, 5 trials; THC oramucosal spray, 3 trials; and oral THC, 1 trial), while 5 trials evaluated synthetic THC (i.e., nabilone). All but 1 of the selected primary trials used a placebo control, while the remaining trial used an active comparator (amitriptyline). The medical condition underlying the chronic pain was most often related to a neuropathy (17 trials); other conditions included cancer pain, multiple sclerosis, rheumatoid arthritis, musculoskeletal issues, and chemotherapy-induced pain. Analyses across 7 trials that evaluated nabiximols and 1 that evaluated the effects of inhaled cannabis suggested that plant-derived cannabinoids increase the odds for improvement of pain by approximately 40 percent versus the control condition (odds ratio [OR], 1.41, 95% confidence interval [CI] = 0.99–2.00; 8 trials). The effects did not differ significantly across pain conditions, although it was not clear that there was adequate statistical power to test for such differences.Only 1 trial (n = 50) that examined inhaled cannabis was included in the effect size estimates from Whiting et al. (2015). This study (Abrams et al., 2007) also indicated that cannabis reduced pain versus a placebo (OR, 3.43, 95% CI = 1.03–11.48). It is worth noting that the effect size for inhaled cannabis is consistent with a separate recent review of 5 trials of the effect of inhaled cannabis on neuropathic pain (Andreae et al., 2015). The pooled ORs from these trials contributed to the Bayesian pooled effect estimate of 3.22 for pain relief versus placebo (95% CI = 1.59–7.24) tested across 9 THC concentrations. There was also some evidence of a dose-dependent effect in these studies.Primary LiteratureIn the addition to the reviews by Whiting et al. (2015) and Andreae et al. (2015), the committee identified two additional studies on the effect of cannabis flower on acute pain (Wallace et al., 2015; Wilsey et al., 2016). One of those studies found a dose-dependent effect of vaporized cannabis flower on spontaneous pain, with the high dose (7 percent THC) showing the strongest effect size (Wallace et al., 2015). The other study found that vaporized cannabis flower reduced pain but did not find a significant dose-dependent effect (Wilsey et al., 2016). These two studies are consistent with the previous reviews by Whiting et al. (2015)and Andreae et al. (2015), suggesting a reduction in pain after cannabis administration.Discussion of FindingsThe majority of studies on pain cited in Whiting et al. (2015) evaluated nabiximols outside the United States. In their review, the committee found that only a handful of studies have evaluated the use of cannabis in the United States, and all of them evaluated cannabis in flower form provided by the National Institute on Drug Abuse that was either vaporized or smoked. In contrast, many of the cannabis products that are sold in state-regulated markets bear little resemblance to the products that are available for research at the federal level in the United States. For example, in 2015 between 498,170 and 721,599 units of medical and recreational cannabis edibles were sold per month in Colorado (Colorado DOR, 2016, p. 12). Pain patients also use topical forms (e.g., transdermal patches and creams). Thus, while the use of cannabis for the treatment of pain is supported by well-controlled clinical trials as reviewed above, very little is known about the efficacy, dose, routes of administration, or side effects of commonly used and commercially available cannabis products in the United States. Given the ubiquitous availability of cannabis products in much of the nation, more research is needed on the various forms, routes of administration, and combination of cannabinoids.CONCLUSION 4-1 There is substantial evidence that cannabis is an effective treatment for chronic pain in adults.
Read MorePsilocybin Mushrooms: A promising companion
Magic mushrooms are undergoing a transformation from illicit recreational drug to promising mental health treatment. Numerous studies have reported positive findings using psilocybin—the mushrooms' main psychoactive compound—for treating depression as well as smoking and alcohol addiction, and for reducing anxiety in the terminally ill. Ongoing and planned studies are testing the drug for conditions that include opioid dependence, PTSD and anorexia nervosa.This scientific interest, plus growing social acceptance, is contributing to legal changes in cities across the U.S. In 2020 Oregon passed statewide legislation decriminalizing magic mushrooms, and the state is building a framework for regulating legal therapeutic use—becoming the first jurisdiction in the world to do so. For now psilocybin remains illegal and strictly controlled at the national level in most countries, slowing research. But an international push to get the drug reclassified aims to lower barriers everywhere.After a flurry of research in the 1950s and 1960s, psilocybin and all other psychedelics were abruptly banned, partly in response to their embrace by the counterculture. Following the 1971 United Nations Convention on Psychotropic Substances, psilocybin was classed in the U.S. as a Schedule I substance—defined as having “no currently accepted medical use and a high potential for abuse.” Psilocybin production was limited, and a host of administrative and financial burdens effectively ended study for decades. “It's the worst censorship of research in history,” says David Nutt, a neuropsychopharmacologist at Imperial College London. Despite these legal hurdles, the current research resurgence has seen Nutt and others exploring how psilocybin changes the brain's connectivity patterns: reducing connections within the usual networks while increasing links between less connected regions. Just this year a study showed that treatment involving psilocybin led to sustained network alterations, which seemed to correlate with reduced depression symptoms. Two organizations are beginning final rounds of trials for psilocybin's use for depression, which could lead to the substance's first approval by the U.S. Food and Drug Administration.As news of psilocybin's promise spreads, several U.S. cities have passed measures decriminalizing magic mushrooms. This is not the same as legalization; the molecule and the mushrooms themselves remain illegal, but prosecuting people for their possession or use is deprioritized or discouraged.In 2019 Denver voters passed a ballot measure that prohibits using city money to prosecute people for magic mushroom–related offenses. City councils soon took similar steps in Oakland and Santa Cruz in California and in Ann Arbor, Mich. In November 2020 voters in Washington, D.C., passed a ballot measure making natural psychedelics one of law enforcement's lowest priorities. Cities and counties in Michigan, Massachusetts, California and Washington State have followed suit.As part of Oregon's legislation, the state health authority created a scientific advisory board to recommend regulations for psilocybin service centers, such as designating mushroom species and preparations to use and production standards to follow. These centers, which can apply for licenses starting next January, will not claim to treat depression but will aim to improve general well-being.“My worry is that people won't necessarily get that distinction ... and turn up with horrible, treatment-resistant depression, expecting an expert in treating that condition,” says Johns Hopkins University psychiatrist Natalie Gukasyan, who led a recent psilocybin trial. Oregon's advisory board is determining how best to train facilitators and screen clients for risk factors, such as a family history of schizophrenia or bipolar disorder. “All our decisions revolve around consumer safety,” says Oregon State University mycologist Jessie Uehling, who chairs the board's product subcommittee. “We want to know that we're avoiding all the potential risks and creating the safest environment for people.” The centers will focus on fungi and natural preparations rather than the synthetic psilocybin used in clinical trials so far, Gukasyan notes.Regardless of local decriminalization, U.S. researchers must still abide by federal Schedule I regulations. The International Therapeutic Psilocybin Rescheduling Initiative, a coalition of research and advocacy organizations, aims to get the World Health Organization to conduct a review of the relevant evidence for reclassifying the drug. “It's inconceivable the WHO could now say psilocybin doesn't have medical value. It can work where other drugs have not,” Nutt says.Various laws already facilitate research and treatment in some countries. Canada classifies magic mushrooms as Schedule III, so penalties are lower, and certain research and trials are granted exceptions. A Canadian charity called TheraPsil has a fast-track process for end-of-life psilocybin therapy. Some countries such as Jamaica never made magic mushrooms illegal, although the psilocybin molecule often is. Research is limited in most of these places, but many have thriving “psychedelic retreat” industries that are not medically regulated. The Netherlands has specifically banned the mushrooms—but its laws don't mention the psilocybin-containing lumps of underground material that eventually sprout them, better known as truffles. This loophole has paved the way for numerous therapeutic retreats, but little organized research.Portugal has famously decriminalized all drugs. Some countries ban the mushrooms but not their spores, because the latter do not contain psilocybin. Others simply do not enforce their laws on magic mushrooms. The 1971 U.N. treaty has a clause allowing countries to exempt traditional Indigenous uses of psychedelic plants. Indigenous people in some South American countries have used psychedelics for centuries and have fought governments for their right to engage in related ceremonies. There is even a religious organization in New Mexico, the Oratory of Mystical Sacraments, that claims members can legally use magic mushrooms in certain circumstances.“This idea that psilocybin is helpful for mental health conditions is not a new one. There are thousands of years of history of efficacious treatment; it's just in a different knowledge format,” Uehling says. “We're trying hard here in Oregon to honor that knowledge system.”Public perceptions of psilocybin are changing, and as increasing interest generates more evidence, this trend looks set to accelerate. “It's a thrilling time to be a mycologist,” Uehling says. Many are waiting to see what happens in Oregon, she adds: “Other states will come up with variations on—hopefully—what we get right, and also on what needs to be changed.”
Read More